Non-Surgical Treatments
Conservative Care for Lasting Spine Health
As most patients do not require surgical intervention, we offer multiple approaches for the care of spinal disorders. We understand that neck and back pain are life-altering conditions and that each patient is an individual with specific needs. Our conservative care options include Pain Management, Physical Medicine and Rehabilitation, Physiotherapy and Chiropractic Medicine. Their goal is to decrease pain and enhance performance without surgical intervention.
Our physicians specialize in the following non-surgical care:
Cervical Epidural injections
Radiofrequency ablation
Vertibroplasty
Kyphoplasty
Epidural injections
Facet Injections
Trigger-point injections
Radiofrequency Ablation
Select Nerve Root Blocks (SNRB)
Intracept Procedure
EMG/NCV
Dry Needling
Acupuncture
Anti-inflammatory Medications (NSAIDS)
Antidepressants or anticonvulsants
Muscle relaxers
Narcotic Medications
Spinal Cord Stimulator
Decompression therapy
Decompression table
Ultrasound therapy
Prehabilitation
Post Surgical Physical Therapy
Cervical Epidural injections
A cervical epidural steroid injection (cervical ESI) is an injection of anti-inflammatory medicine, a steroid or a corticosteroid, into the epidural space around the spinal nerves. The main goal is to manage pain caused by irritation and inflammation of the cervical nerve roots. Also known as cervical radiculopathy, this can present as neck pain, arm pain, or weakness.
Radiofrequency ablation
RFA is for the long-term relief of the chronic neck (typically C3-C7), thoracic (typically T5-6), lumbar (typically L3-L5), that originates from facet joints-the small bones of the spine. These joints can become painful from arthritis, injury, or degeneration. Before performing this procedure, a diagnostic medial branch block is done to confirm the pain source. The procedure uses a fluoroscopic guided needle positioned near the small sensory nerves (medial branch nerves) that carry the pain signals from the affected facet joints. Numbing agent is used, and then a controlled radiofrequency current is applied through the needle tip, gently heating and deactivating those pain-transmitting nerves.The pain relief typically lasts 6-18 months, it improves mobility and function, reduces the need for pain medications and only requires 1-2 days of downtime.This procedure does not impact muscle strength or spinal cord function.
Read More: Facet joint syndrome: from diagnosis to interventional management - PMC
Vertibroplasty
Minimally invasive, out-patient, fluoroscopically-guided injection of bone cement into a fractured vertebrae, usually done under anesthesia, to immediately stabilize and relieve pain. This is done for compression fractures caused by osteoporosis, trauma or metastatic cancer, that have not improved with rest, bracing, or medications. It can be life-changing for patients needing pain relief, improved mobility, and to prevent further collapse of fractured bone.It takes less than an hour and offers pain relief within 24-48 hours.This procedure is similar to kyphoplasty, however kyphoplasty uses a balloon and restores lost vertebral height.
Kyphoplasty
Minimally invasive, out-patient procedure, typically done under anesthesia, to treat compression fractures, usually caused by osteoporosis, trauma or spinal tumors, This procedure involves a fluoroscopically-guided needle being injected into the fractured vertebra. A tiny balloon is gently inflated to restore height, and this creates a cavity inside the bone, which is then injected with bone cement, which hardens and stabilizes the fractures. It takes less than an hour and offers pain relief within 24-48 hours. Regular activities can start shortly after completing the procedure. The benefits of this procedure are rapid pain relief, improved spinal stability, correction of spinal alignment and vertebral height, improved posture, and reduced need for pain medications.
Epidural injections
A lumbar epidural steroid injection (Lumbar ESI) is an injection of anti-inflammatory medicine-a steroid or corticosteroid- into the epidural space around the spinal nerves. The main goal is to manage chronic pain caused by irritation and inflammation of the spinal nerve roots in your low back, which can be due to certain conditions or injuries. This type of chronic pain is called lumbar radiculopathy, and it can radiate down from your back to your hips, legs and or feet.
Facet Injections
Medication is injected directly into the joint, and is also called an intra-articular facet joint. These injections can also be used to diagnose the source of pain, as a positive response would indicate that the facet joint is the source of the pain.
Trigger Point Injections
(TPIs) are a treatment that involves injecting a local anesthetic or other substance into a muscle trigger point to relieve pain and relax muscles. They are thought to temporarily relax the muscle and, which can improve blood flow, and break the pain cycle. They are used to treat myofascial pain, which can include chronic or episodic headaches, back pain, and temporomandibular joint pain. TPIs can be combined with corticosteroid or numbing agents such as lidocaine, or with no substance (dry needling), and they can be administered not more frequently than every three months.
Radiofrequency Ablation
RFA is for the long-term relief of the chronic neck (typically C3-C7), thoracic (typically T5-6), lumbar (typically L3-L5), that originates from facet joints-the small bones of the spine. These joints can become painful from arthritis, injury, or degeneration. Before performing this procedure, a diagnostic medial branch block is done to confirm the pain source. The procedure uses a fluoroscopic guided needle positioned near the small sensory nerves (medial branch nerves) that carry the pain signals from the affected facet joints. Numbing agent is used, and then a controlled radiofrequency current is applied through the needle tip, gently heating and deactivating those pain-transmitting nerves.The pain relief typically lasts 6-18 months, it improves mobility and function, reduces the need for pain medications and only requires 1-2 days of downtime. This procedure does not impact muscle strength or spinal cord function.
Select Nerve Root Blocks (SNRB)
These are used both to diagnose and treat pain caused by irritation or inflammation caused by a specific spinal nerve. The procedure is used when there are pain symptoms radiating such as sciatica, arm pain or numbness to pinpoint the nerve root responsible (e.g. mapping the pain to L4 versus L5). These steroid injections can also reduce inflammation and pain along the irritated nerve pathway. SNRB injections differ from epidurals in that they are given to specific nerve roots rather than the entire epidural space. The pain relief may start within a few days, and diagnostic information is usually evident within 24 hours.
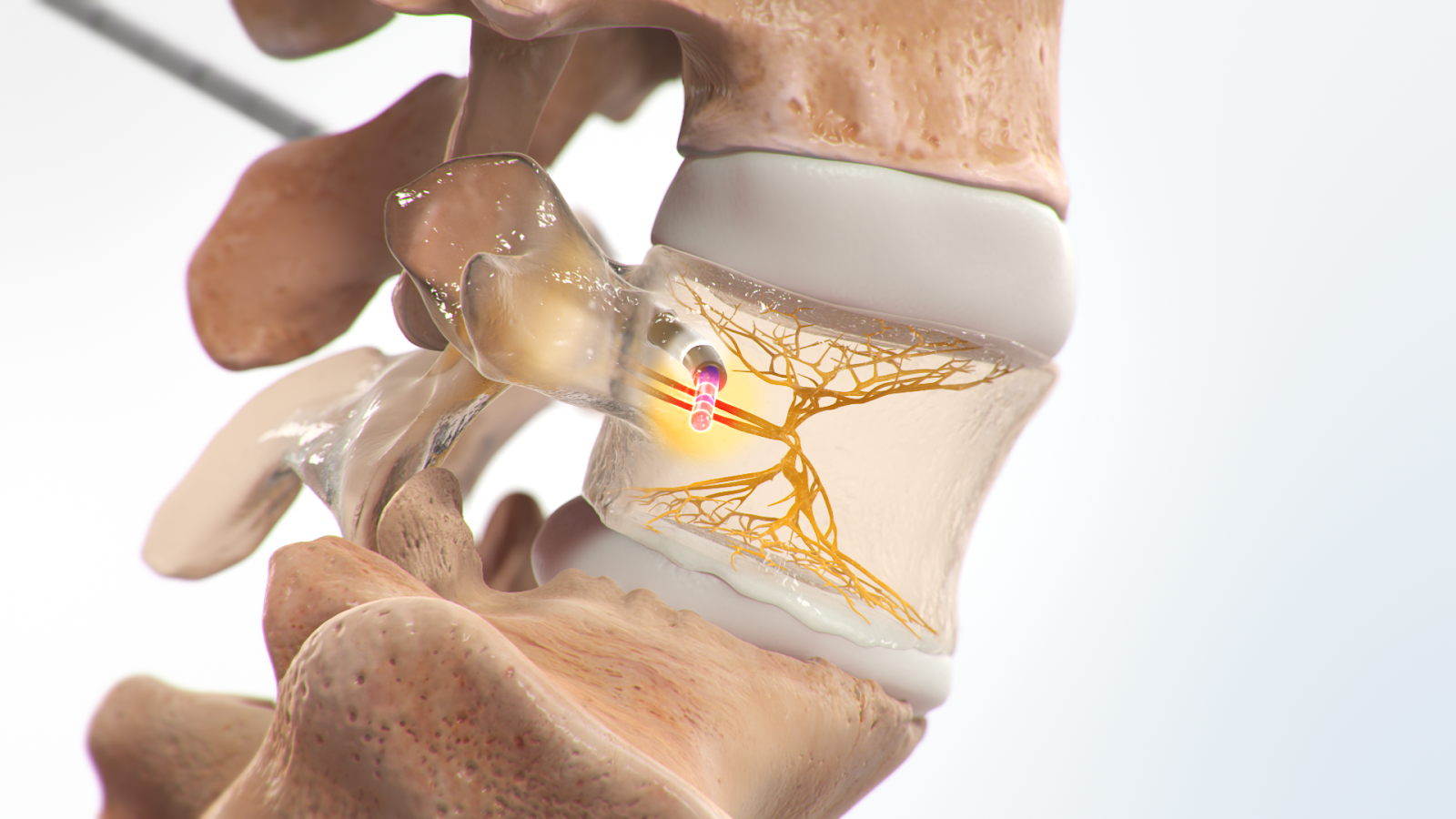
Intracept Procedure
Overview: this procedure is a minimally invasive, image-guided treatment designed to relieve chronic low back pain that originates from the vertebral endplates-vertebrogenic pain. It targets the basivertebral nerve (BVN), a small nerve that transmits pain signals with radiofrequency energy to deactivate this nerve inside the vertebral body. A small cannula is positioned in the vertebral body, then a radiofrequency probe is inserted to target the basivertibral nerve using targeted thermal ablation to prevent the nerve from transmitting pain signals.
Indications: This is for patients with chronic low back pain unresponsive to PT, injections and medications, with Modic type 1 or type 2 changes as seen on an MRI (commonly L3-S1). This type of axial low back pain presents as deep aching, worse with sitting, bending or prolonged standing.
Benefits:Minimally invasive, performed on an outpatient basis,allows for a rapid recovery. It targets vertebrogenic pain, rather than just symptoms, with results lasting beyond 5 years.
Recovery: Patients return home the same day with mild soreness at the insertion site. Regular activities can resume within a couple of days. Improved pain and function are typically seen after 2-6 weeks.
Caveat: This procedure requires MRI correlation with Modic changes, as it treats pain from the vertebral body, versus discs, facet joints, or nerve compression.
EMG/NCV
Electromyogram and nerve conduction testing are used to diagnose neuro-muscular disease. These typically include carpal tunnel syndrome, but also peripheral neuropathy, radiculopathy, and brachial plexopathy. EMG testing involves the placement of a sterile needle and takes approximately one hour to complete. NCV testing involves surface electrodes on the skin. Both studies are targeted to presenting symptoms and specific nerves to be tested.
Facet Injections:
Dry Needling
In our office this treatment is done by a physical medicine physician with specialized training. It treats musculoskeletal pain and movement issues, and acts as an adjunct with a larger pain management program. Thin sharp needles are used to puncture the skin and deeper tissue, muscle and connective tissue, to treat myofascial trigger points. The goal is to relieve pain and improve movement by causing microlesions, which trigger the body’s natural healing response. No medication is injected.
Acupuncture
This ancient therapeutic technique originates from Chinese medicine and is used to treat pain and restore physiological balance. At our clinic, acupuncture is done by a pain management physician. It serves as a complimentary, non surgical modality to modulate pain pathways, reduce muscle spasm, and enhance patient wellbeing in particular those with chronic neck or back pain, radiculopathy or post operative discomfort.The practise involves very fine needles inserted into specific anatomical points, acupoints, that correspond to areas where nerves, muscle, and connective tissue can be stimulated to influence local blood flow and neurochemical activity.This adjunct therapy serves to restore function, minimize pain and optimize overall patient outcomes.
Medications:
Anti-inflammatory Medications (NSAIDS)
This includes drugs such as Naprosyn, Motrin, and Celebrex. This medication is non-addicting and will help with inflammation in the body. Prescription anti-inflammatory medication should not be taken with over-the-counter medications such as Aspirin, Motrin, Nuprin, Advil, Aleve or Excedrin. Note that Tylenol is not an anti-inflammatory and can be taken along with the anti-inflammatory medication.
The most common side effect of anti-inflammatory medication is stomach upset, including ulcers. Stop the medication if you develop nausea, heartburn, stomach upset or any other adverse effect.
Antidepressants or anticonvulsants
Medications such as amitriptyline or gabapentin can help manage nerve pain (neuropathic pain).
Muscle relaxers
This includes drugs such as Carisoprodol, Flexeril (cyclobenzaprine), Robaxin (methocarbamol, zanaflex (tizanidine), and Skelaxin. These medications can cause drowsiness, and using this medication in the evening is recommended, or at times when you do not need to drive, and or do activities that require sharp thinking abilities.
Narcotic Medications
This medication is habit-forming/ addicting, constipating, and can cause drowsiness/depressed mood. We only use this medication short-term to help with pain control. It should not be taken with alcohol or other medication that may cause drowsiness.
Pain Procedures:
Spinal Cord Stimulator
Spinal cord stimulators consist of thin wires or electrodes placed between the spinal cord and the vertebrae or epidural, and a battery pack or generator placed under the skin. The patient can then send electrical impulses when they feel pain, using an external remote control.
The mechanism behind the pain relief is not clearly understood. It is known that the brain’s sense of pain is altered. The placement of this device is done by a physician with specialized training.
Chiropractic Treatment and Manual Therapy:
Decompression Therapy
Often referred to as spinal decompression therapy, is a non-surgical treatment aimed at relieving pain associated with disc issues, sciatica, and other spinal conditions. Here are some potential benefits:
Pain Relief: It can help alleviate chronic back pain, neck pain, and radicular pain by reducing pressure on spinal discs and nerves.
Improved Mobility: Patients often experience increased range of motion and improved flexibility in the spine.
Disc Hydration: The therapy may promote better hydration of spinal discs, potentially aiding in their health and function.
Reduced Need for Surgery: For some individuals, this therapy can be an alternative to invasive surgical procedures.
Enhanced Healing: By creating a negative pressure in the discs, it may help promote the healing of herniated or bulging discs.
Non-Invasive: It is a non-surgical option, making it less risky compared to surgical treatments.
Decompression Table
Patients suffering from the chronic pain of bulging, degenerating, or herniated discs may benefit from treatment using a decompression table. This type of pain can manifest as back and neck, and even leg and arm pain. Using computerized sensors to perform stretching actions on the spine to promote healing can be uniquely effective.
Ultrasound Therapy
A therapeutic treatment that uses sound waves to promote healing and reduce pain in various musculoskeletal conditions. It utilizes high-frequency sound waves (typically between 1 and 3 MHz) that penetrate the skin and underlying tissues. It can produce thermal effects (increasing tissue temperature) and non-thermal effects (such as promoting cellular activity and tissue repair). The procedure is done with a handheld transducer to deliver ultrasound to the targeted area.
Benefits: UT therapy can reduce inflammation and promote relaxation in affected areas. It can also increase blood flow and encourage tissue regeneration. Many patients experience improved flexibility and range of motion following UT. And lastly it can help resolve post surgical adhesions and scar tissue.
Indications: It is used for muscle strains, bursitis and tendonitis, both chronic and acute. It aids in the recovery after surgery to address soft tissue inflammation.
Caveat: although the procedure is safe when done by a professional, it may not be safe for everyone (e.g.implants), and treatment may require multiple sessions for optimal results.
Prehabilitation
Why is prehabilitation important?
Rehab before surgery is crucial in developing endurance and strength in the muscles so when minimally invasive surgery occurs muscles can handle being retracted. Postsurgical rehab is a lot easier when previous surgical rehab has been provided. There is less chance to have muscle injuries when muscles are endurance.
Post Surgical Physio Therapy
Why have chiropractic care and physical therapy?
Research shows that chiropractic care with physical therapy was beneficial compared to just chiropractic care or just physical therapy. Chiropractic can help keep mobilization in joints that have decreased mobility. Chiropractic adjustments with exercise help to keep the joint functioning properly.


Making spine care easy and convenient for Canadians
Please call or text us at 602-953-9500 to schedule your consult