Surgical Procedures
Nobody Knows Your Spine Like We Do
Today’s Technology
Top experts using the most advanced technologies and advancements in medicine.
Leaders in Spine Surgery
Board-certified and fellowship-trained surgeons & experienced staff.
Our physicians specialize in the following surgical procedures:
Minimally Invasive Surgery
Anterior Lumbar Interbody Fusion (ALIF)
Posterior Lumbar Interbody Fusion (PLIF)
Transforaminal Lumbar Interbody Fusion (TLIF)
Lateral Lumbar Interbody Fusion (XLIF)
Laminectomy
Discectomy
Scoliosis/Deformity
Cervical Disc Replacement
Cervical Discectomy and Fusion
Endoscopic Spine Surgery
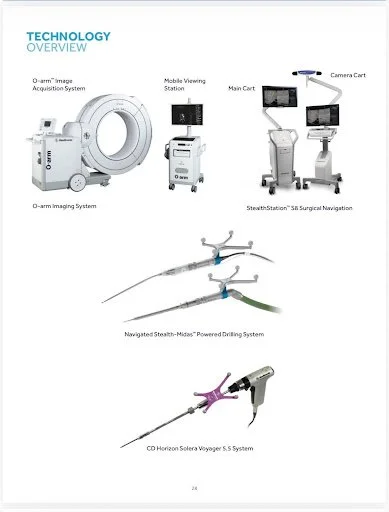
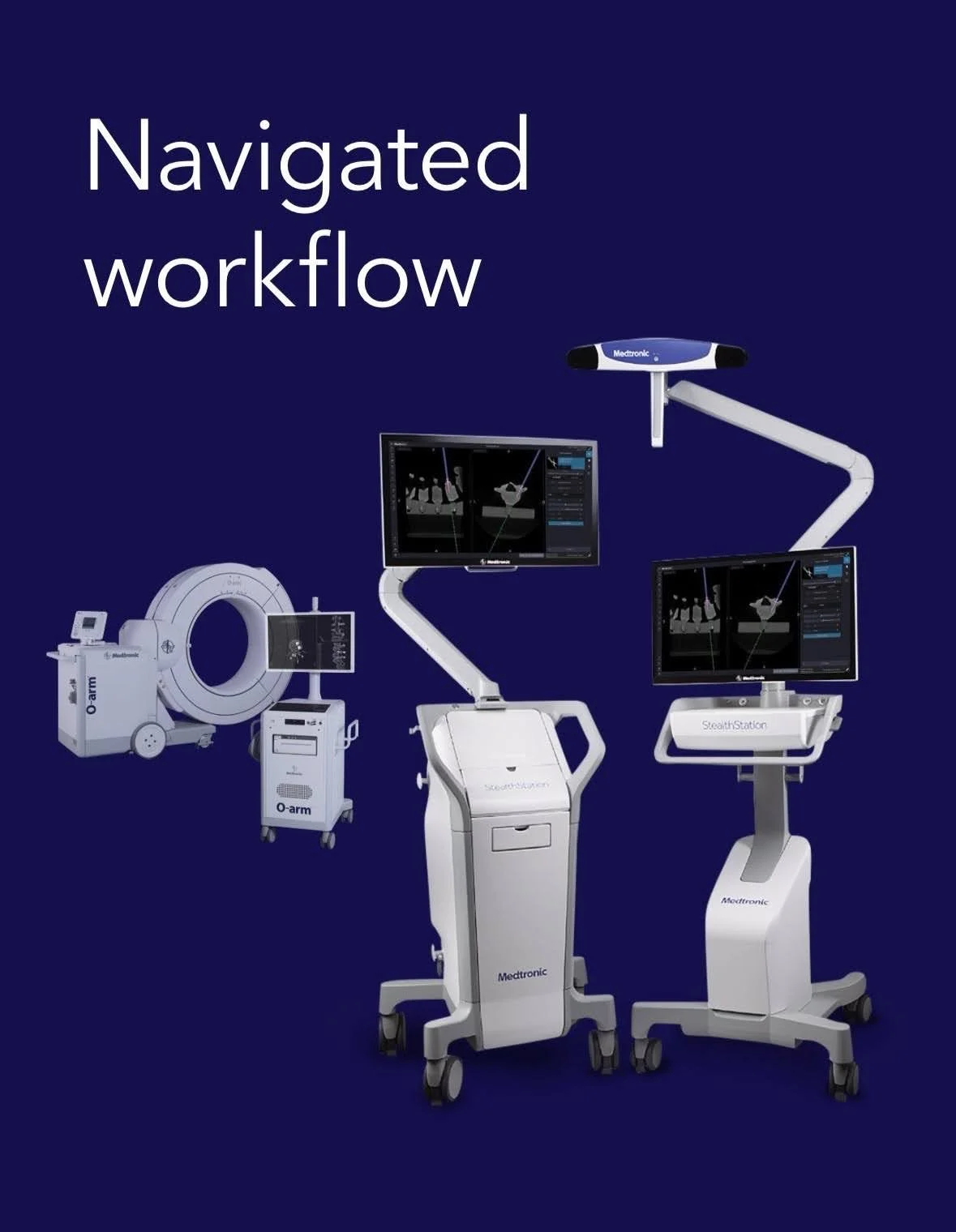
Navigated and robotic-assisted spine surgery
SI Joint Fusion
-
This minimally invasive procedure involves the use of screws or triangular dowels to stabilize the joint and alleviate pain at the sacroiliac joint. It is typically performed through a small minimally invasive lateral incision, using image guidance. The objective is to fuse the sacrum to the ilium.
-
For patients with chronic, refractory SI joint pain who have successfully received pain relief with diagnostic injections and failed appropriate physical therapy.. Some conditions are SI joint arthritis, degenerative sacroiliitis, instability due to trauma, prior lumbar fusion, inflammatory conditions, sacral insufficiency, or adjacent segments disease post spine surgery.
-
This procedure is a minimally invasive approach, reducing operative time, blood loss, and it uses a smaller incision. Reduces pain and improves function within weeks for most patients, improves joint stability, and restores alignment.
-
Patients typically spend a few hours in the hospital and then return home. Weight-bearing may be limited on the operated side for several weeks, and a walker may be used. PT is prescribed after the initial healing period to restore strength, flexibility, and gait mechanics. Light activity can resume at 2-4 weeks, and full activity post joint fusion is 3-6 months.
Lumbar Total Disc Replacement (TDR)
-
This is a surgical procedure to remove a diseased or degenerated lumbar intervertebral disc and replace it with an artificial disc implant. Unlike traditional spinal fusion, TDR preserves motion at the operated disc segment.
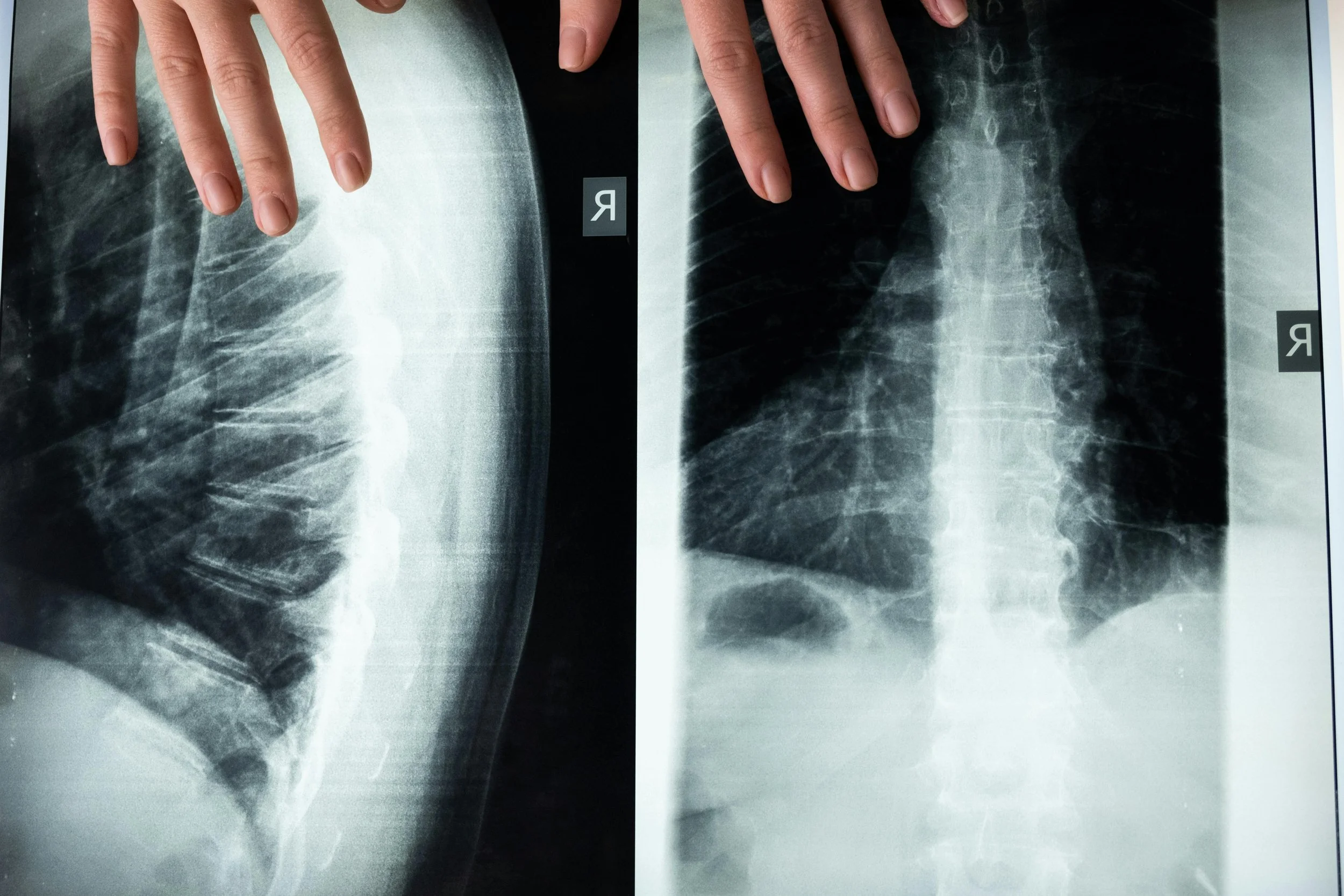
Imaging studies (x-ray, MRI, CT) are used to identify the degenerated disc level, assess spinal alignment, and rule out contraindications such as severe facet joint disease. In surgery, the patient is positioned supine for an anterior (front) approach for direct access to the disc space. The diseased intervertebral disc is carefully removed, preserving surrounding bone and ligaments. The artificial disc is sized and inserted into the disc space; it’s designed to replicate motion while maintaining disc height and spinal alignment. The incision is closed, typically leaving a small anterior abdominal scar.
-
This may be recommended for patients with degenerative disc disease causing chronic low back pain, pain limited to one or two disc levels without significant facet joint arthritis, failed conservative management, and no significant spinal instability, osteoporosis or spondylolisthesis.
-
TDR preserves motion at the operated segment versus spinal fusion, reduces the stress on adjacent segments, potentially lowering the risk of adjacent segment disease, it is effective for pain relief for some degenerative disc patients, it restores disc height and spinal alignment, improving posture and nerve space, the minimally invasive anterior approach results in a smaller incision and less muscle disruption versus the posterior fusion surgery.
-
A typical hospital stay is 1-3 days. Walking the day of surgery is recommended; sedentary activities can resume 2-4 weeks, and physically demanding activities can resume at 6 weeks. PT begins within a few weeks to restore core strength and spinal stability. Most patients achieve maximum pain relief and mobility at 3-6 months. Regular follow-up imaging ensures proper implant position and spinal alignment.
Minimally Invasive Anterior Cervical Spine Discectomy and Fusion
-
This is a surgical procedure performed on the cervical spine (neck) from the front. The surgeon makes a small incision in the front of the neck, typically in the natural skin folds, to minimize scarring. The muscles, blood vessels, and other soft tissues are gently moved aside to expose the cervical spine. A damaged or herniated disc is removed, all or part. The surgeon may then insert a bone graft (from the patient, a donor, or synthetic material) between the vertebrae to encourage them to fuse, stabilizing the spine. Depending on the procedure, screws, plates, or other hardware may be used to stabilize the spine during the healing process.
-
This procedure can be done for cervical disc herniation, cervical spondylosis (DDD), spinal stenosis, fractures or dislocations, and tumors.
-
This provides relief of nerve compression, which can alleviate pain, weakness, or numbness in the neck, shoulder, arms, or hands. Spinal alignment and function is improved, leading to improved quality of life. The risk of permanent nerve damage or disability is also reduced.
-
Surgery is typically done as an outpatient. A cervical collar or brace may be used for several weeks to support the neck during healing. PT is often recommended to restore the range of motion and strength. Full recovery can take several months, although many patients experience significant symptom relief within weeks.
Posterior Cervical Fusion
-
procedure performed from the back (posterior) of the neck to relieve pressure on the spinal cord and or nerve root or to stabilize the cervical spine. It can involve removing bone or soft tissue (Laminectomy – removal of the lamina, the roof of the vertebra) to enlarge the canal, or Foraminotomy – enlarging the foramen where nerves exit. Posterior cervical decompression and fusion is the most common (PCDF or PCF). If fusion is required, it involves screws and rods for stability, and a bone graft or bone graft substitute to promote fusion.
-
When conservative treatments have failed or when there is progression of neurologic symptoms, cervical fusion can be done for cervical spinal stenosis, cervical radiculopathy, cervical instability, cervical tumors, and infections that require decompression and stabilization, and also for multilevel degenerative disc disease when several levels are affected, making an anterior approach less effective.
-
The possible benefits include the relief of the symptoms caused by spinal cord and nerve compression, such as neck and arm pain, decreased hand coordination, balance, and strength, as well as stopping further neurologic decline. Also improved stability in cases of spinal instability and deformity, and better overall function and quality of life.
-
Typically, this requires a 1-3 day hospitalization, depending on the number of cervical levels addressed. Initial recovery, the first few weeks, there is pain and stiffness, which are controlled with medications. A neck brace may be worn for several weeks to support healing. Walking and light activity are encouraged early. Heavy lifting should be avoided, as well as overhead reaching and sudden neck movements. During the intermediate recovery period, 6-12 weeks, a gradual increase in activity and physical therapy starts. Desk work is permitted at 2-4 weeks, and physical jobs take 3-6 months. The full bone fusion takes between 3 months to one year, and most patients have lasting pain and functional improvements, particularly if surgery is completed before significant nerve or spinal cord damage occurs.
-
Cervical artificial disc replacement surgery (arthroplasty) is a motion-preserving surgical procedure that involves removing a diseased cervical disc and replacing it with an artificial disc. The discs are the cushions that lie between the vertebrae. They act as shock absorbers and allow your neck to move freely. These discs can break down, lose their height, and their cushioning effect. They can also become displaced and compress the spinal cord or the nerve roots. This can cause neck pain, upper extremity pain, numbness, weakness, or tingling. This minimally invasive surgery can be used to treat one or two-level disease, and there are several implants on the market that are FDA approved. (animation****). The procedure is typically performed through a minimally invasive anterior (front) approach to the neck, allowing direct access to the cervical spine. Under general anesthesia, a 2-3 cm incision is made along the front of the neck to expose the cervical vertebrae. The degenerative or herniated disc is completely removed, decompressing the spinal cord and nerve root. The space is prepared for the artificial disc prosthesis.
-
Cervical disc arthroplasty is indicated for patients with cervical disc herniation or degenerative disc disease that is causing radiculopathy (arm pain, numbness, weakness) or mild myelopathy, and conservative treatment with PT, medications, and injections have failed. This can be done at a single level or two levels between C3 and C7. Adequate bone quality and stability are needed, without significant facet joint degeneration.
-
This surgery allows for motion preservation of the cervical spine and reduces adjacent segment degeneration. The recovery is faster with less stiffness than with a fusion surgery, and the implant provides immediate stability.
-
This surgery allows for motion preservation of the cervical spine and reduces adjacent segment degeneration. The recovery is faster with less stiffness versus a fusion surgery, and the implant provides immediate stability.
-
Most patients are discharged from the hospital within 24 hours. Postoperative discomfort is typically mild. Early gentle neck motion is encouraged; a soft collar can be used for comfort. Light activities can begin at 1-2 weeks, and normal activity can begin at 4-6 weeks.
-
Patient selection is critical, as success depends on addressing neural compression while maintaining healthy facet joints and alignment.
Cervical Disk Arthroplasty (disc replacement)
Cervical Laminoplasty
-
Cervical Laminoplasty is a surgical procedure performed to relieve pressure on the spinal cord caused by cervical spinal stenosis, a condition where the spinal canal in the neck narrows and compresses the spinal cord. Unlike spinal fusion, cervical laminoplasty is a decompression surgery aimed at expanding the spinal canal to create more space for the spinal cord and nerves, while preserving motion in the cervical spine. An incision is made on the back of the neck (posterior approach). Muscle and soft tissue around the spine are moved aside to expose vertebrae and laminae (bone arches of the vertebrae that form the back of the spinal canal). The lamina is partially removed to relieve pressure on the spinal cord, this is the laminectomy, which serves to reshape the size of the spinal canal to create more space for the spinal cord. Bone spurs or disc material may also be removed. Laminoplasty, the reshaping and stabilizing of the lamina, involves reshaping the bony structure in a way that opens up the spinal canal. Often, the lamina is hinged, or “flipped” to create a broader canal. In some cases, the lamina may be secured in place using small metal plates, screws, or sutures to hold it in an expanded position and ensure the spinal canal remains open for the spinal cord and nerve roots.
-
Cervical laminoplasty is typically performed when there is cervical spinal stenosis with myelopathy (spinal cord compression). This can be caused by degenerative disc disease, cervical spondylotic myelopathy, trauma, and congenital stenosis, which can worsen with age.
-
Decompression relieves the pressure on the spinal cord and nerve roots to resolve pain, numbness, weakness, and walking difficulties. This surgery allows for the preservation of motion, unlike a spinal fusion, which permanently restricts movement between the affected vertebrae. Laminoplasty preserves motion in the cervical spine. This is especially important in younger, more active patients who wish to maintain a natural range of motion in the neck. This surgery can reduce the likelihood of further degeneration of adjacent segments. This is a highly successful surgery for decompression and symptom relief, especially in patients with cervical myelopathy due to degenerative conditions.
-
Most patients stay in the hospital for 1-2 days after cervical laminoplasty. Some patients may need to wear a neck brace or collar for a short period to provide stability while healing. Postoperative pain is usually mild to moderate and can be managed with medications and ice packs. Physical therapy is prescribed within a few weeks of surgery to help restore strength, flexibility, and range of motion in the neck. Most patients are advised to avoid heavy lifting or strenuous activities for a few weeks to allow the spine to heal properly. Full recovery, including return to normal activities, typically takes 6-12 weeks.
-
Cervical laminoplasty is an effective surgical option for treating cervical spinal stenosis and related conditions that cause spinal cord compression. It provides pain relief and improves neurological function with a lower risk of adjacent segment degeneration compared to spinal fusion.
Minimally Invasive Deformity Surgery for Scoliosis
-
This surgical approach is to correct spinal curvature (scoliosis) using smaller incisions (versus traditional), muscle-sparing techniques, and specialized instrumentation. The surgery involves detailed imagery (x-ray, MRI, CT) to measure the spinal curves, identify rigid segments, and plan the screw placement. The patient is placed in a prone position on a radiolucent table with access to the spine .A small incision is made to the affected vertebrae, using specialized instruments and retractors to gently move muscles. Pedicle screws are inserted into the vertebrae, and rods are placed for the instrumentation segments, stabilizing the spine permanently. Incisions are then closed with minimal tissue disruption to reduce scarring and postoperative pain.
-
This surgery is done when conservative management with PT, medications and injections fail to resolve back and leg pain. It is done for adult and degenerative scoliosis and adolescent idiopathic scoliosis.
-
The include smaller incision, less tissue trauma, faster recovery and shorter hospital stay, reduced blood loss, effective correction and spinal stabilization, lower risk of infection and complications, and preservation of surrounding muscles and ligaments.
-
Typical hospital stay is 3-5 days, depending on the number of levels addressed. Patients begin walking the day after surgery. Physical therapy is initiated within a few weeks to restore strength and flexibility. Light activities can be resumed within 4-6 weeks, and more strenuous activity over 3-6 months. The fusion timeline is generally 6-12 months. Physician follow-up is needed to ensure proper hardware placement and spinal alignment.
Ultra Minimally Invasive Lumbar Endoscopic Surgery
-
The endoscopic technique utilizes a slender, camera-equipped instrument that grants surgeons a clear view to navigate the spine's intricate pathway through incisions 5 times smaller than conventional and 3 times smaller than minimally invasive tubular surgical incisions. This refined technique is particularly beneficial for individuals enduring persistent back and/or leg symptoms that defy non-surgical treatments who want to return to their life, work, and hobbies quickly and safely.
-
An ultra-minimally invasive surgical approach to address a variety of spinal conditions, including herniated discs and spinal stenosis.
-
Endoscopic spine surgery can minimize muscle and local tissue collateral injury all the while affording excellent access to the pathology causing insult. Numerous randomized-controlled studies observed the same quality outcomes in pain and function at intermediate- and long-term follow-up, with the advantage that this procedure leads to reduced immediate postoperative pain, shorter hospital stays, and accelerated recovery times compared to open spine surgery.
-
Endoscopic spine surgery is unique to each individual. Many patients can resume activities within a few weeks after their surgery. Patients typically experience less pain and a faster recovery compared to traditional surgery. They may be able to return to normal activities within a few weeks, although complete healing may take several months.
Endoscopic Lumbar Discectomy / Decompression
This procedure is performed to decompress the spinal canal by removing a small portion of the lamina (the bony roof over the spinal canal) and any compressive soft tissue using endoscopic visualization and specialized instruments. This surgery relieves pressure on the spinal canal and nerve roots while preserving normal anatomy and minimizing soft tissue trauma.
-
MRI and CT scans are used to localize the level of the spinal stenosis or nerve compression and determine the best surgical approach. The patient is positioned face-down (prone) on a radiolucent table to allow fluoroscopic guidance. A small incision is made over the affected level, the endoscope and camera with high-definition magnified visualization of the surgical field as seen on the monitor, are then used to remove part of the lamina, ligamentum flavum, and any bony spurs or herniated disc material compressing nerves The goal is to free the affected nerve root, while maintaining as much of the normal bone and joint structure as possible. The incision closure only requires one or two sutures or adhesive strips.
-
This is used for patients with lumbar spinal stenosis causing leg pain, numbness, or weakness, lumbar disc herniation with nerve root compression, lateral recess or foraminal stenosis, recurrent stenosis after prior surgery, and failure of conservative treatment such as medication, injections, and PT.
-
This surgery has a very small incision, which limits muscle disruption, reduces postoperative pain and narcotic use, shortens hospital stay, faster recovery, lowers risk of infection and blood loss, preservation of normal spinal stability, and enhances visualization during the procedure for a precise decompression.
-
Surgery is typically outpatient, ambulation is within hours after the surgery, return to sedentary activity in 1-2 weeks, and more physical activity in 4-6 weeks. PT begins 2-3 weeks post-op to improve flexibility and core strength.
Read More on Endoscopic Spine Surgery
Minimally invasive anterior lumbar fusion (ALIF)
-
ALIF is a surgical procedure to fuse one or more lumbar spine segments from the front (anterior) of the body. It provides direct access to the intervertebral disc through a small incision in the abdomen, allowing disc removal, restoration of the spinal alignment, and placement of a bone graft or interbody cage (spacer), while minimizing disruption to the back muscles. Imaging, including X-rays, MRI, and CT, are used to evaluate the spinal anatomy, disc height, vascular structures, and surgical level. The patient is positioned on their back (supine) to allow access to the lumbar spine from the front. A small abdominal incision is made, with the retraction of muscles, vessels, and abdominal organs to expose the spine. The degenerated intervertebral disc is removed, endplates of the adjacent vertebrae are prepared for the fusion cage (spacer). The incision is closed with minimal tissue disruption.
-
ALIF may be recommended for patients with degenerative disc disease causing chronic low back pain, spondylolisthesis (vertebral slippage), loss of disc height or lumbar lordosis leading to poor spinal alignment, failed conservative treatments, and patients requiring multilevel lumbar fusion.
-
The anterior approach allows for complete disc removal and placement of larger interbody cages, it restores disc height and spinal alignment, improving posture and nerve decompression, this minimally invasive approach reduces back muscle disruption versus posterior fusion, it reduces blood loss and postoperative pain versus the posterior approach, has lower risk of adjacent segment disease due to restoration of natural spinal alignment, and can be combined with percutaneous posterior instrumentation for additional stability if needed.
-
Typical hospital stay is 1-3 days, early activity such as walking begins the day after surgery, return to sedentary activities can resume 2-4 weeks, and physically demanding activity can begin 8-12 weeks. PT is initiated within a few weeks to restore core strength and improve mobility. The fusion timeline is generally 3-12 months.
Minimally Invasive Posterior Lumbar Fusion: Transforaminal Lumbar Interbody Fusion (TLIF)
-
The minimally invasive procedure involves removing damaged discs between the vertebrae and fusing the vertebrae to stabilize the spine. The "transforaminal" part of the name refers to the surgical approach, which accesses the spine through the posterolateral region, the side, in an area called Kambin's Triangle, or the "foramen,” to minimize disruption to surrounding tissues like muscles and nerves. During a TLIF, the surgeon will remove the affected disc material and replace it with a bone graft and spacer (Cage) to help the vertebrae fuse over time, in addition to screws and rods.
-
TLIF is done for patients with degenerative disc disease, spondylolisthesis, spinal stenosis, herniated discs, and spinal instability. TLIF is considered when non-surgical treatments (such as physical therapy, medications, or injections) have not provided sufficient relief, and surgery is necessary to improve stability and reduce pain.
-
This surgery reduces abnormal motion at a degenerated or unstable disc level and decreases pain and nerve compression. It further reduces degeneration of the surrounding segments, restores disc height, can reduce mild spinal deformities, and protects the spinal nerves from irritation and compression. The TLIF approach from the posterior minimizes surgical trauma to spinal muscles and ligaments compared to a traditional posterior fusion: less blood loss, smaller incision, and less postoperative muscle trauma. The surgical approach also allows direct access to the disc space and spinal canal. It preserves midline bony structures and ligaments, and maintains spinal integrity and reduces post op pain. The procedure can be done at a single or multiple levels
-
Most patients will undergo a Minimally Invasive TLIF (MIS TLIF) at an outpatient facility and go home the same day. Depending on medical comorbidities, some surgeries may be done in the hospital and require an overnight stay. Some patients may be instructed to wear a back brace to support the spine during the early stages of recovery. Expect some pain and discomfort after surgery, but medications will help manage this. Your doctor will guide you on transitioning off stronger medications. Physical therapy may be prescribed after a few weeks, and walking is recommended within the first few days. In the short term, sitting for periods longer than 30 minutes is discouraged, as is bending, lifting, and twisting. Full recovery can take up to 6-12 months for the fusion to solidify.
Minimally Invasive Direct Lateral Fusion (XLIF, DLIF)
-
Lateral lumbar interbody fusion, also called DLIF, LLIF, or XLIF, is a minimally invasive spinal fusion surgery performed through a small incision on the side of the torso. This procedure allows access to the side of the lumbar spine without disrupting major back muscles or the spinal canal, to remove damaged intervertebral disc material and stabilize the spine with a cage (spacer) filled with bone graft. The affected disc level and any nerve compression are identified by x-ray, MRI, or CT. The patient is positioned side-lying, and an incision is made through the flank using specialized instruments to separate muscles to reach the side of the vertebra. The damaged intervertebral disc is partially or fully removed, and the implant, a spinal cage filled with bone graft, is placed in the disc space to restore disc height and maintain spine alignment. The implant is fixed with lateral screws or posterior pedicle screws, and the small incision is closed across the muscle and skin.
-
degenerative disc disease causing chronic back pain, spondylolisthesis, degenerative scoliosis, failed conservative management, and cases of recurrent disc herniation or spinal instability.
-
Minimally invasive procedure with a smaller incision, less muscle dissection, and reduced blood loss. Faster recovery versus an open fusion surgery, reduced post-operative pain versus posterior surgical approach, improved spinal alignment with regard to lordosis and disc height, lower risk of infection and complications due to smaller surgical exposure.
-
The hospital stay is typically 1-2 days, depending on co-morbidities. Most patients can walk the same day, and light activity and physical therapy begin within days. Sedentary activities can begin at 2-4 weeks, and heavier activities can take 8-12 weeks. The bone fusion occurs over 6-12 months. Pain control, PT, and bone health (calcium and vitamin D) are important for recovery.
Lumbar Total Disc Replacement (TDR)
-
This is a surgical procedure to remove a diseased or degenerated lumbar intervertebral disc and replace it with an artificial disc implant. Unlike traditional spinal fusion, TDR preserves motion at the operated disc segment.
Imaging studies (x-ray, MRI, CT) are used to identify the degenerated disc level, assess spinal alignment, and rule out contraindications such as severe facet joint disease. In surgery, the patient is positioned supine for an anterior (front) approach for direct access to the disc space. The diseased intervertebral disc is carefully removed, preserving surrounding bone and ligaments. The artificial disc is sized and inserted to the disc space; it’s designed to replicate motion while maintaining disc height and spinal alignment. The incision is closed, typically leaving a small anterior abdominal scar.
-
May be recommended for patients with degenerative disc disease causing chronic low back pain, pain limited to one or two disc levels without significant facet joint arthritis, failed conservative management, and no significant spinal instability, osteoporosis, or spondylolisthesis.
-
TDR preserves motion at the operated segment versus spinal fusion, reduces the stress on adjacent segments, potentially lowering the risk of adjacent segment degeneration, it is effective for pain relief for some degenerative disc patients, it restores disc height and spinal alignment, improving posture and nerve space, the minimally invasive anterior approach results in a smaller incision and less muscle disruption versus the posterior fusion surgery.
-
Typical hospital stay is 1-3 days, walking the day after surgery is recommended, sedentary activities can resume 2-4 weeks, and physically demanding activity can resume at 6-12 weeks. PT begins within a few weeks to restore core strength and spinal stability. Most patients achieve maximum pain relief and mobility at 3-6 months. Regular follow-up imaging ensures proper implant position and spinal alignment.
Percutaneous SI Joint Fusion
-
This minimally invasive procedure involves the use of screws or triangular dowels to stabilize the joint and alleviate pain at the sacroiliac joint. This is typically performed through a small incision, using image guidance. The objective is to fuse the sacrum to the ilium.
-
For patients with chronic, refractory SI joint pain who have successfully received pain relief with diagnostic injections. Some conditions are SI joint arthritis, degenerative sacroiliitis, instability due to trauma, prior lumbar fusion, inflammatory conditions, sacral insufficiency, or adjacent segment disease post-spine surgery.
-
This procedure is a minimally invasive approach that reduces operative time, blood loss, and requires a smaller incision. Reduces pain and improves function within weeks for most patients, improves joint stability, and restores alignment.
-
Patients typically spend a few hours in the hospital and then return home. Weight-bearing is limited on the operated side for several weeks, and a walker may be used. PT is prescribed after the initial healing period to restore strength, flexibility, and gait mechanics. Light activity can resume at 2-4 weeks, and full activity post joint fusion is 3-6 months.

Making spine care easy and convenient for Canadians
Please call or text us at 602-953-9500 to schedule your consult